Learn about our Inpatient Clinical Dataset, including key outcome measures, how to collect the dataset, data compliance, submission, audit and reporting, and supporting documents.
Inpatient dataset
Inpatient Clinical Dataset
- The rehabilitation benchmarking initiative
- The AROC clinical datasets
- Data collection forms
- The outcome measures
- How to collect the inpatient clinical dataset
- Data compliance, submission, audit and reporting
AROC was established with a main goal of improving clinical rehabilitation outcomes by benchmarking rehabilitation providers in Australia and New Zealand. AROC commenced in 2002 with an inpatient data collection and provides benchmarking through reports and specialist workshops. Rehabilitation services participating in AROC routinely collect the AROC dataset and submit their data to the AROC Database. This data is combined and analysed by AROC and used to provide a suite of benchmarking reports which allow services to benchmark themselves with their peers. The ultimate goal of the initiative is to improve rehabilitation outcomes across Australia and New Zealand.
The AROC clinical datasets have evolved through consultation with rehabilitation providers and representatives of peak organisations from across Australia and New Zealand. Where possible, National Health Data Dictionary definitions have been used.
The AROC Version 4 dataset was realeased in July 2012 following review and update. The AROC Version 4 clinical dataset comprises a “bank” of data items pertaining to episodes of rehabilitation care. The three inpatient (admitted) pathways (models of care) are;
Inpatient direct care (Pathway 3)
- rehabilitation is delivered in an inpatient setting
- the patient is accommodated overnight in the hospital and included in the bed occupancy reporting at midnight
- the patient is under the care of the rehabilitation physician who holds the medical governance/ bed card
In-reach (Pathway 2)
- the patient is under the care of an acute physician who holds the medical governance/bed card
- the rehabilitation physician or team 'reaches into the acute setting to begin the process of rehabilitation in addition to the acute care the inpatient is already receiving
Consult / Liaison (Pathway 1)
- The patient is under the care of one physician who holds the medical governance / bed card and another physician or team provide a one-off consultation service
Access the AROC version 4 clinical data dictionaries. These provide information about each of the data items in the AROC data bank.
History of the inpatient dataset
The AROC version 1 clinical dataset commenced in July 2002 and was based on the rehabilitation dataset that was used in the 2007 AN-SNAP study and was still being collecting by many rehabilitation facilities. This was soon revised and replaced with the AROC version 2 clinical dataset in September 2003. Both version 1 and 2 of the AROC clinical dataset enabled the collection of ambulatory data, however, the focus was on the inpatient collection.
In July 2007 the AROC clinical dataset was split into two: version 3 inpatient and version 1 ambulatory. The inpatient clinical dataset introduced new items forward, trauma, complications as well as fields for the generation of the ACHS Clinical Indicators (to save time for member facilities participating in the ACHS accreditation process). Items such as the AROC impairment code, comorbidities, level of support received, employment status, onset date and rehabilitation suspensions were also updated.
Access the data collection forms for the version 4 dataset are available by pathway and country. These will assist in ensuring that all the relevant data items are collected for data entry. The proformas are available in Microsoft Word format and can be modified to suit the needs of participant services as desired.
Key outcome measures used by AROC include, but are not limited to:
Functional Independence Measure (FIM)
The choice of functional outcome measure in the inpatient setting through all clinical datasets has been the FIM as the focus of inpatient rehab is on a return to physical and cognitive functional ability in the self care spectrum. The FIM instrument assesses an individuals activity limitations and their need for assistance (or burden of care) to perform basic life activities. The functional ability of a patient changes during rehabilitation and the FIM instrument is used to track those changes. Functional change is a key outcome measure of rehabilitation episodes. .
Length of stay (LOS)
The length of stay (LOS) of a rehabilitation episode is the number of days on which care has been provided. It is calculated as the rehabilitation end date (date discharged from rehabilitation service) minus the rehabilitation start date (date admitted to the rehabilitation service), minus the number of leave days during the rehabilitation episode of care. Many rehabilitation patients will also have had an acute LOS prior to their rehabilitation episode – this is not included in the rehabilitation LOS.
LOS and FIM change benchmarks
Each reporting period AROC publishes national and sector benchmarks by impairment and AN-SNAP class. The first benchmarks for New Zealand data were published in the 2008/2009 financial year. In Calendar Year 2014 AROC introduced the benchmarks specific for brain dysfunction and spinal cord dysfunction split into specialist and non-specialist. In Calendar Year 2015 AROC updated the benchmarks to include analysis by AN-SNAP class V4.
FIM efficiency
The change in functional status from the beginning to the end of the rehabilitation episode is measured by the change in FIM score. This is calculated as the FIM score at the end of the episode minus the FIM score at the start of the episode. FIM efficiency is then this average change in FIM score per day. This statistic is calculated as the mean change in FIM score divided by the mean length of stay (LOS). The higher the value the greater the level of functional improvement per day.
Discharge destination
The type of accommodation before and after an episode of rehabilitation are collected to reflect and compare where the patient has come from (what was their usual accommodation) and where they are going to. The final destination may be defined as the accommodation that a patient is discharged to that is the most appropriate long term accommodation for the patient with the goal being to return them back to their usual accommodation from prior to rehabilitation. For patients not able to return to the most ideal accommodation immediately post discharge even though their rehabilitation is deemed complete an interim accommodation may be used. This scenario may indicate complexity of the patients’ discharge, or the lack of equipment and/or services available to the patient.
Facilities can choose to:
- Enter their inpatient data directly into the AROC database using the AROC Online Services (AOS) online data entry system, or
- Enter their data into their own IT systems, with the AROC V4 clinical dataset items built in. AROC data extracts are then extracted from the IT system and uploaded to AROC via the AROC Online Services (AOS) online data upload system, for inclusion in the AROC database.
All items in all AROC clinical datasets are mandatory and should be collected and submitted to AROC via AROC Online Services (AOS). It is important that all uploaded data conform to the specified format of the AROC extract, therefore, if a facility is unable to collect some items in the AROC data set space for them should be included in their data extract.
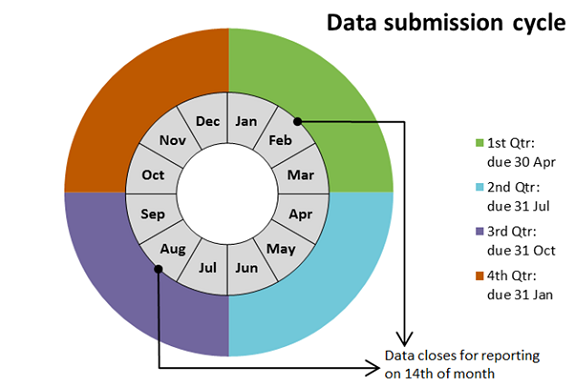
Data is expected to be submitted quarterly to AROC, however many facilities submit their data monthly.
Facilities using AOS Data Entry are given error checks at the point of data entry, and can print the individual patients audit report and/or summary page for case meetings.
For facilities uploading data to AROC the process is iterative. First facilities create an AROC data extract using their data entry system based on episode discharge dates. Then upon uploading their data extract into AOS they receive a data audit, and are given the opportunity to amend their data, if required. Once corrected the data are again extracted and uploaded to AROC, to undergo the same process. This process of error checking may be required to happen multiple times until the data are free of errors or the facility determines that any remaining errors cannot be fixed.
Following data submission AROC runs benchmark reports twice a year:
- Calendar year: Jan 1 – Dec 31 period (Reporting data closes Feb 14)
- Financial year: Jul 1 – Jun 30 period (Reporting data closes Aug 14)
After the closing date for the reporting data, inpatient data are concatenated, data items for reporting are calculated (e.g. AN-SNAP class, length of stay, age on admission, FIM total scores) and then individualised benchmark reports are generated for participating services.