March 13, 2014
Anti-inflammatories could be used to fight superbugs, researchers say
Researchers in Wollongong have discovered that some common anti- inflammatory drugs have an antibiotic effect, suggesting they may have a role to play in treating the ‘superbugs’ that pose a major risk to human health.
In research published today (13 March) in the prestigious Cell Press journal, Chemistry & Biology, Illawarra Health and Medical Research Institute (IHMRI) researchers based at the University of Wollongong found that several non-steroidal anti-inflammatory drugs (NSAIDs) act on bacteria in a way that is fundamentally different from current antibiotics, which may open up new strategies for fighting drug-resistant infections.
The “chance discovery” was made while the researchers were working on an Australian Research Council grant to develop antibacterial agents targeting a critical protein in DNA replication and repair.
“We were developing inhibitors of a specific protein in bacteria called the DNA clamp, which is essential to ensure DNA replication and cell proliferation,” explains the paper’s lead author, Associate Professor Aaron Oakley.
“These sliding DNA clamps, which are conserved across bacterial species, sit on the DNA like a ring to prevent other proteins which are essential for DNA replication and repair from wandering off. While testing specific compounds that would bind to the clamp and prevent it from interacting with its binding partners, we noticed that one compound had a similar molecular structure to carprofen, an anti-inflammatory widely used in veterinary medicine.
“So we tested carprofen and two other common NSAIDs [vedaprofen and bromfenac] and found they had an antibiotic effect on gram-positive and gram-negative bacteria such as E. coli. In effect, they prevented the bacteria from copying their DNA.”
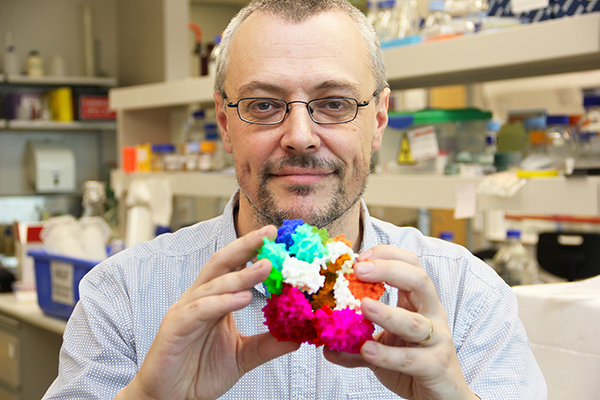
Associate Professor Oakley has since used 3D printing technology to build a 3D model of the DNA clamp and the common binding site at which these new antibacterial agents are targeted (see attached image).
The research team, which includes Professor Nick Dixon, Dr Michael Kelso and Professor Jenny Beck, also from UOW’s School of Chemistry, will now concentrate on getting the NSAIDs to bind to the site more tightly and recently applied for a National Health and Medical Research Council grant to pursue this line of enquiry over the next three years.
“While our research is a long way from clinical trials, the fact that the bacteria-killing effects of the anti-inflammatories is different from conventional drugs means that they could be developed into new kinds of antibiotics,” adds Associate Professor Oakley.
“This is important given the fact that the superbugs have become resistant to many, and in some cases most, of the available antibiotics. We do consider this a breakthrough that will capture a lot of attention among our colleagues. It is one of those serendipitous encounters that scientists live for.”
Media contacts: Associate Professor Aaron Oakley is available for interview on +61 420 205 891 or aarono@uow.edu.au. For more information, contact IHMRI Communications Coordinator, Robyn Gower, +61 2 4252 8228 or rgower@uow.edu.au.