June 19, 2018
Patriarchs on pedestals? How doctors are taught to improve their bedside manner
Student doctors need good role models to learn good patient communication.
Up until around 30 years ago, in the days of paper patient files, doctors were on pedestals and patients generally did as they were told, in a more patriarchal model of patient care. Over 2,400 years ago, Hippocrates wrote:
The physician ought also to be confidential, very chaste, sober, not a winebibber, and he ought to be fastidious in everything, for this is what the profession demands.
Since Hippocrates, bedside manners have varied greatly. From low points during early 18th century England, when a motley crew of physicians, barber surgeons, apothecaries and quacks “treated” patients with dirty hands and instruments, selling a range of useless powders and potions, to the more austere and conventional late Victorian age, as medicine progressed towards being one of the most universally respected professions.
Before the first wide-scale use of effective antibiotics from the 1940s, it has been said that medical history was for the most part the history of placebos. The art of medicine, incorporating bedside manner, was often all that either doctor or patient could rely on.
Read more: How doctors are taught to deal with death
Today, medical professionals are technocrats, consulting with the help of software packages linked to powerful databases and search engines. Patients rightly expect doctors to listen to their health concerns, do appropriate physical examinations and tests, and provide up to date, expert treatment advice.
We recognise a successful consultation with our doctor when we leave the surgery with a practical solution to our problem and a vibe that we have been an equal and respected partner in making health decisions.
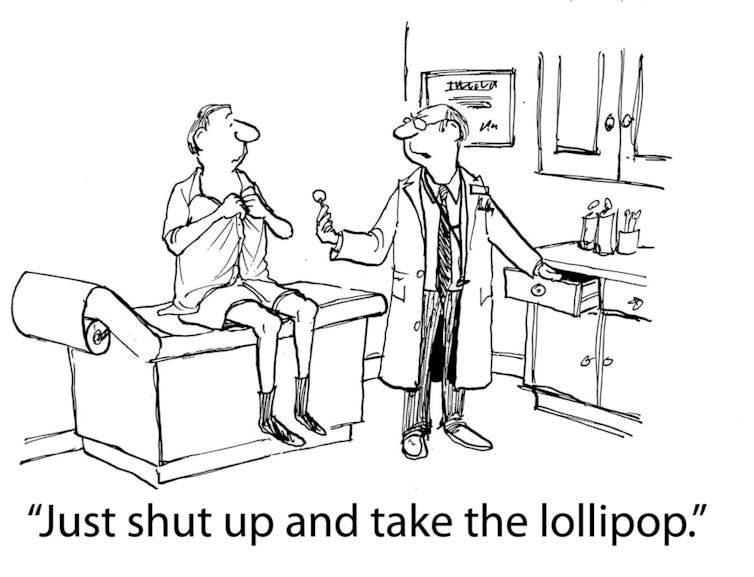
Likewise, we know what happens when it all goes terribly wrong: the doctor didn’t listen, you were rushed through the consultation, or you were given some medication but little in the way of advice.
Teaching doctor communication
Medical students are taught a lot about communication during their studies. At my university for example, from year one of the graduate medical program, students are given regular feedback on ideal “doctor-patient” interactions from clinical teachers and from “standardised patients”, the hundreds of community volunteers from all walks of life who play the role of patients at the medical school.
Medical students are taught the skills with which to put their patient at ease, to take a comprehensive history relevant to the problem, and how to explore the biological, psychological and social aspects of a particular health issue for that person. Beginning from when the patient walks in, students are taught to employ open body language, polite and friendly introductions to establish rapport, to reassure regarding confidentiality, and to structure their questions in a logical and sensitive manner.
Even in their final year clinical examinations, 10% of the marks given to each student are from standardised patients, based on how likely they felt it was they would want to see the student again as their doctor.
Read more: Female doctors show more empathy, but at a cost to their mental well-being
There’s also evidence good bedside manner can benefit the patient, either from care that aims to build positive expectations, or from emotionally supportive care.
A study of patients with high blood pressure told to expect a higher repeat blood pressure reading revealed higher levels than those of similar patients told their second reading would be the same or reduced.
Studies of patients with breast cancer have identified a number of beneficial effects of doctors’ positive communication style. Providing treatment choice, involving patients in decision making, or touching the patient’s hand and providing support, may reduce long term anxiety and depression, contribute to higher quality of life, or even improve physical functioning.
Later in the medical course, students observe their clinical teachers to get a better grasp on patient communication. It’s vital students have excellent modelling of care for a patient in distress, or the considered, compassionate breaking of bad news to a patient.
How much empathy is too much?
This role modelling can be a double-edged sword. Many experienced doctors have evolved superb knowledge, skill and empathy towards their patients, and provide wonderful role models. However, as with any profession, there can also be negative role modelling, which can have a powerful impact on professional development, including bedside manner.
There is some evidence that as medical students evolve into medical professionals, they may experience an erosion of empathy.
Read more: Are our busy doctors and nurses losing empathy for patients?
The quandary for medical educators, and individual doctors, is how to develop the best balance of empathy with clinical competence. An ability to temporarily suppress empathy may assist the doctor’s brain to perform high level cognitive tasks and to emotionally detach while managing complex medical problems.
The practical ability of a surgeon operating on a brain aneurysm is obviously paramount, if they were thinking about their empathy for the patient in this moment they would not be able to perform in surgery. Another part of the puzzle is that, over time, risk of burnout and negative mental health effects may be greater for more empathetic doctors.
![]() In future, a growing number of therapeutic and medical investigation options, the plethora of information driving patient and doctors’ choices, and growth in the alternative medicine industry, are all likely to test doctors’ bedside manner. Medical educators need to be good role models for incoming doctors, to ensure our future doctors feel happy and our patients feel cared for.
In future, a growing number of therapeutic and medical investigation options, the plethora of information driving patient and doctors’ choices, and growth in the alternative medicine industry, are all likely to test doctors’ bedside manner. Medical educators need to be good role models for incoming doctors, to ensure our future doctors feel happy and our patients feel cared for.
Mark Wilson, Associate professor, University of Wollongong
This article was originally published on The Conversation. Read the original article.
UOW academics exercise academic freedom by providing expert commentary, opinion and analysis on a range of ongoing social issues and current affairs. This expert commentary reflects the views of those individual academics and does not necessarily reflect the views or policy positions of the University of Wollongong.
:format(jpg)/prod01/channel_3/assets/live-migration/www/images/content/groups/public/web/media/documents/mm/uow248449.jpg)